Pancreas biopsy
Percutaneous pancreas biopsy is a procedure that is in fact quite easy and safe although interventionalists are generally reluctant to do it due to some concerns. There is a risk of hemorrhage in pancreatic biopsy, but the risk of serious bleeding in experienced centers is only about 1%, and in such a case, the bleeding vessel can be closed easily by embolization (blockage of the bleeding vessel in the angio suit) without surgery. Passing of thin biopsy needles through the stomach and small intestine is not usually a problem, but with a meticulous technique, it is usually possible to place the biopsy needle without passing through these organs. As with all needle biopsies, pancreatic biopsy has a risk of seeding the tumor cells through the hole through which the needle passes, but in many studies this risk was found to be only one in ten thousand. In conclusion, percutaneous pancreatic biopsy has a low-risk and high-accuracy (over 90%) and should be the first line biopsy technique for suspicious pancreatic masses.
How is it done?
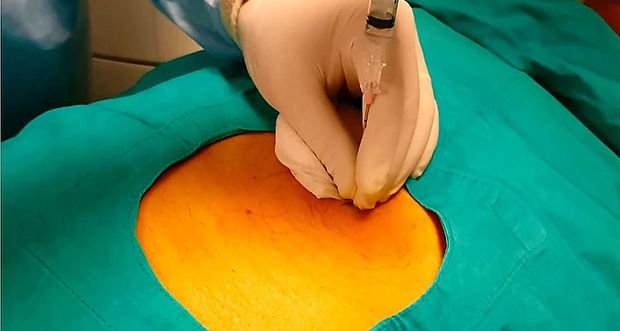
Pancreas biopsy can be performed under ultrasound or CT guidance. After the skin entry site is numbed with local anesthesia, a needle is advanced into the pancreatic mass. Care should be taken not to pass through the vessels around the pancreas, the large intestine, stomach and small intestine. For this, it is important that these structures are well visualized on CT and ultrasound. In experienced hands, pancreatic biopsy is a safe and painless procedure that can be completed in about 10 minutes.
Pancreatic biopsy can be also done with endoscopic ultrasound (EUS). However, the accuracy of this method is lower than percutaneous biopsy, and since only cells are aspirated (not tissue samples), further pathologic studies such as immunhistochemistry and genetic test can not be performed. In contrast, since percutaneous biopsy obtains original tissue samples, both the diagnostic accuracy is higher and further tests can be performed which may help determine the type of cancer, and best possible treatment option.
In some centers, pancreatic biopsy is done via surgical operation. This situation is explained to the patient that both biopsy and surgery will be performed in one time. However, pancreatic surgery is a severe operation with a risk of death and serious complications. If a patient with a suspicious mass in the pancreas has undergone surgery biopsy and the result is benign, the patient will have been unnecessarily operated. Even if the mass is cancer, 85% of the patients will not have any benefit from the surgery, but will have to face the risks and problems of the surgery. Therefore, surgical biopsy in pancreatic masses should only be performed as a last resort if needle biopsy cannot be performed or is unsuccessful.
Video information: "Tomography-guided pancreatic biopsy"

Interventional oncology in cancer management
Prof Saim Yilmaz, MD


